Mysteries of sleep: insights and discoveries
An interview with Professor William Wisden, Imperial College London, conducted by Hyewon Kim
From a chance encounter with a review article on histamine and wakefulness, to leading a research group investigating the fundamental purpose of sleep, Professor William Wisden shares in this interview some intriguing findings. Discussions on brain clearance during sleep and its implications for conditions like dementia prompt even more questions.
What sparked your interest in studying sleep?
It was kind of an accident. My work on sleep began purely by chance, though still within neuroscience. Before that I had worked on various other molecular neuroscience topics, including cloning of neurotransmitter receptors for GABA and glutamate. In the middle part of my career I was focused on the cerebellum and motor learning, but it was a saturated field, and I was looking for a change. While at the University of Heidelberg, where I organized the speaker program, I randomly came across a review article about histamine and wakefulness while flipping through a hard copy of Nature Neuroscience. The author, Prof. Helmut Haas was from Heinrich-Heine-University in Düsseldorf, which was relatively close to Heidelberg. So, I invited him down to speak, even though I knew nothing about the topic.
Helmut explained during his seminar how histamine kept the brain awake. Over dinner he discussed problems of sleep, sparking my interest. I was about to take a position in Aberdeen as a professor and Head of Neuroscience when Helmut invited me to a sleep meeting in Düsseldorf. There I encountered many well known sleep researchers and found the topics they presented fascinating. Slowly I started working on sleep, initially by working with a student who developed mice to allow histamine neurons to be genetically targeted.
At that time, I was also studying potassium channels, specifically K2P leak channels, which were targets for anaesthetics. Nick Franks at Imperial College in London – known for his work on anaesthetics – discovered they bind proteins to cause anaesthesia. He wanted to use our knockout mice, and we connected through a mutual colleague. Nick was also interested in sleep. Thus, I began focusing on sleep research in 2009 when I moved to Imperial College London. Nick also shifted his focus to sleep from anaesthetics, and we joined and merged our labs.
How do you define sleep preparatory behaviours?
It is actually an important concept because we are vulnerable when we sleep. A wild animal has to find a secure place or go to its burrow. I feel that this is an essential part of surviving the night or the day when you're sleeping. We need to prepare for sleep in the right way.
What have been some known general or clinical results of disturbed sleep?
There is a condition called narcolepsy, where you go from wakefulness to REM sleep, often triggered by emotion. This condition involves a missing peptide called orexin that promotes wakefulness, and people with narcolepsy often have antibodies against orexin or its receptors.
People with dementia and Parkinson's disease also experience sleep disturbances. Retrospectively, many people who develop Parkinson's have sleep disturbances up to ten years before full symptoms emerged. Sleep issues often mark the onset of illness.
There are also rare conditions where people fall asleep excessively, known as hypersomnia, and illnesses where people are missing sleep, such as in bipolar disorder. During the manic phase, individuals often sleep very little.
Many diseases have disturbed sleep patterns because sleep is so central, and these patterns can be used diagnostically. In addition to narcolepsy, sleep disorders include REM sleep behaviour disorder, where people act out their dreams due to lack of muscle paralysis during REM sleep.
While pure sleep disorders are relatively rare, neurodegenerative diseases cause poor sleep patterns, affecting both patients and caregivers. This isn't a specific sleep disease per se but rather a sign that brain circuits are deteriorating.
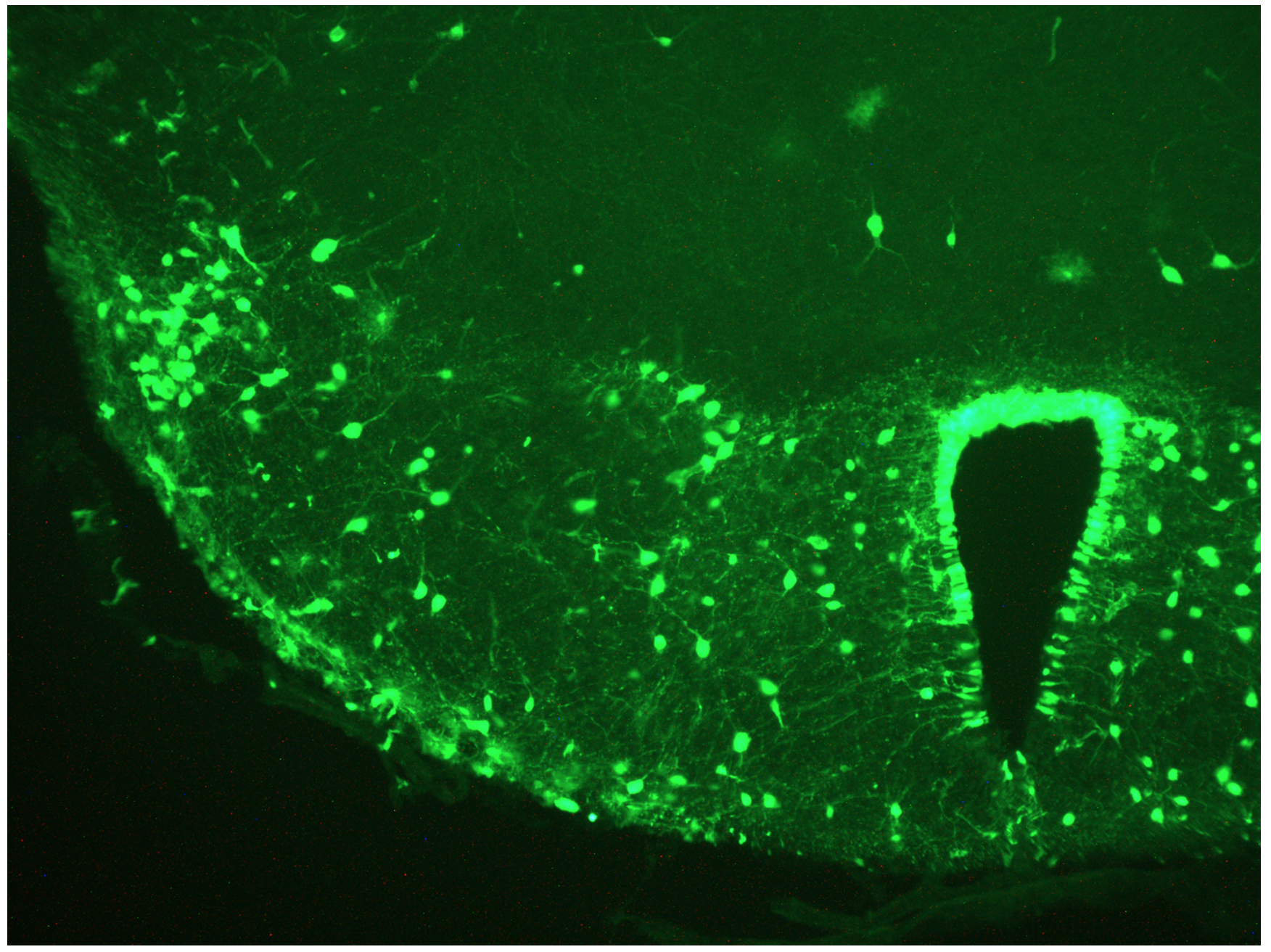
How did you study sleep deprivation and subsequent recovery sleep in mice? Why did you use cFOS?
cFOS is a well-known marker of neural activity. My PhD supervisor Stephen Hunt pioneered its use in the 1980s to study pain pathways. cFOS serves as a surrogate to see if neurons are active and many researchers have used it to mark sets of neurons genetically. This technique has been applied to study memory in the hippocampus. We thought, why not copy that method to study the sleep drive?
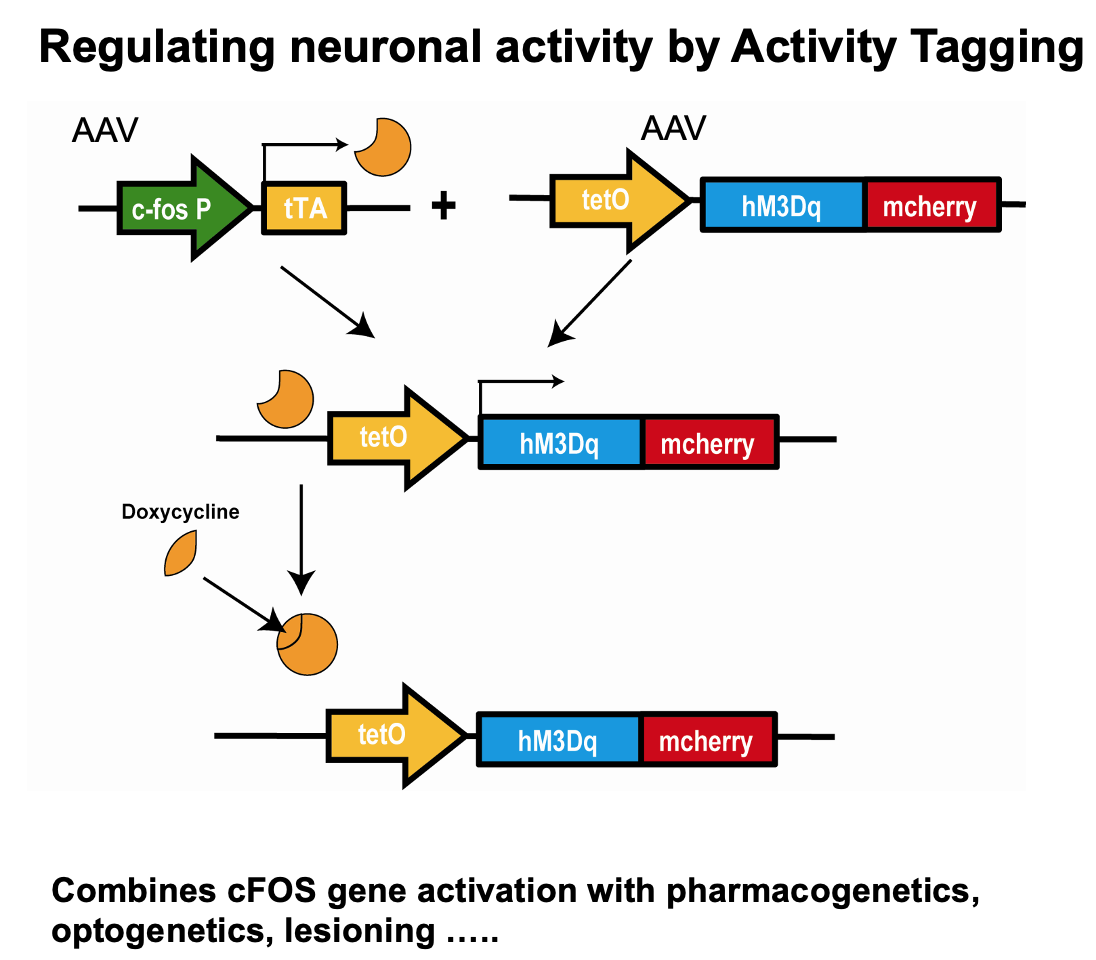
Many researchers had studied sleep using techniques like sleep deprivation and recovery sleep, which are well documented. However, we were the first to think of using cFOS trapping to look at the sleep drive. It seemed like an easy and obvious idea, but for some reason we were the first to apply it to sleep research.
You also found that brain clearance is actually reduced, not helped, by sleep. How do you make sense of this result?
It means clearance is helped by being awake. When you're asleep, that process actually works less well. Clearance works better when we're awake, possibly because you have a higher heart rate or blood pressure – whatever drives the clearance, which is still unknown.
A related question is, why do we need to be unconscious when we sleep? What happens in our bodies that requires us to be switched off? Why can't we regenerate while we're awake, just sitting quietly and talking? It's a mystery of the field. It would have been nicer if clearance had something to do with sleep, given that's what we work on, but that's how we think about it until proven wrong.
Does sleep impairment influence amyloid plaques in the neocortex in the context of dementia?
Other researchers had shown before us that amyloid plaques increase with time spent awake, a well-known finding, for example by David Holzmann and colleagues in St Louis.
On one hand, we showed that the clearance of small molecules works better when awake, but it might be different for molecules like amyloid plaques. It could also be that it's not the actual sleep that matters but rather the reduced time spent awake, giving less opportunity for plaques to build up. Sleep might act as a kind of buffer.
This is a very important area. I definitely think good sleep can help stop dementia-related pathology, but it might be because we spend less time awake. We just don't know yet.
What is your current hypothesis on how the PFC-hypothalamus circuit induces sleep and sleep preparatory behaviours?

Somehow, in an unknown way, a part of the brain senses when it is becoming tired. The important question is to find out what this means metabolically. What is the environment of the neuron that makes it excited and then part of the sleep-promoting circuitry? What drives this tiredness at the brain level?
It's an important question to determine what exactly makes us tired. This is a very fundamental issue,.
In your view, what is the neuroscientific purpose of sleep?
I believe that's one of the most important questions in neuroscience: why do we sleep? Currently, we don't have a good hypothesis. I think there's a basic physiological drive, like hunger, that compels us to sleep. Once we figure it out, it'll probably seem obvious, and someone else might say, "Why didn't I think of that?" It'll be fascinating to look back on. But right now in my opinion, it's not obvious at all.
What are some next steps of your research that you are excited about?
We aim to understand more about clearance and how it works for different types of molecules because it's still unclear how things are cleared from the brain. Additionally, we want to uncover the purpose of sleep, which I believe is our most important goal. Stay tuned for updates on our research!

About Professor Wisden
William (Bill) Wisden studied Natural Sciences (zoology) at the University of Cambridge, and did his PhD with Stephen Hunt at the MRC Molecular Neurobiology Unit, Cambridge, followed by a postdoc with Peter Seeburg at University of Heidelberg. Bill was at the centre of studies characterising gene families for GABA and glutamate receptors. Since 2009, Bill has been at Imperial College London, and in a long-term collaboration with Nick Franks (also at Imperial) he has used mouse genetics to investigate sleep. Bill is a member of the UK Dementia Research Institute.


